No vaccines exist that protect people against infections by coronaviruses, including SARS-CoV-2, which causes COVID-19, or the ones that cause SARS and MERS. As COVID-19 continues to wreak havoc, many labs around the world have developed a laser-like focus on understanding the virus and finding the best strategy for stopping it.
This week in mBio, a journal of the American Society of Microbiology, a team of interdisciplinary researchers describes a promising vaccine candidate against the MERS virus. Since the MERS (Middle East Respiratory Syndrome) outbreak began in 2012, more than 850 people have died, and studies suggest the virus has a case fatality rate of more than 30%.
In the new paper, the researchers suggest that the approach they took for a MERS virus vaccine may also work against SARS-CoV-2. The vaccine's delivery method is an RNA virus called parainfluenza virus 5 (PIV5), which is believed to cause a condition known as kennel cough in dogs but appears harmless to people. The researchers added an extra gene to the virus so that infected cells would produce the S, or spike, glycoprotein known to be involved in MERS infections.
"We know people have been exposed to PIV5, but it seems to be an innocuous virus in humans," said pediatric pulmonologist and coronavirus expert Paul McCray, M.D., at the University of Iowa, in Iowa City, who co-led the new study with virologist Biao He, Ph.D., at the University of Georgia, in Athens. "PIV5 doesn't seem to cause a cytopathic effect." The MERS virus cannot replicate in mice, so to test the vaccine McCray developed a mouse model that mimics human infections. The mice had been genetically engineered to express DPP4, the protein used by the MERS virus as an entry point for human cells.
Lab tests showed that a single dose of the vaccine, given intranasally, effectively caused infected cells to produce the S protein, which in turn triggered immune responses against the protein in the animal host.
Four weeks after the mice received the vaccine, they were exposed to a strain of the MERS virus, adapted to the mice to cause a lethal infection. The MERS virus was also given to groups of mice that had received a different PIV5 vaccine -- one without the genes for the S protein -- or an intramuscular vaccine with inactivated MERS virus.
All the mice immunized with the modified PIV5 virus survived MERS virus infection. In contrast, all the mice immunized with the PIV5 without S died from the infection. The intramuscular vaccine of inactivated MERS virus only protected 25% of the mice from a lethal infection. The mice that received inactivated MERS virus showed above-average levels of eosinophils, white blood cells that indicate infection or inflammation. This connection raises a safety concern for inactivated MERS virus as a potential vaccine, said He. The study demonstrates that an intranasal, PIV5-based vaccine is effective against MERS in mice, said He, and should be investigated for its potential against other dangerous coronaviruses, including SARS-CoV-2.
"We're quite interested in using viruses as gene delivery vehicles," said McCray, who has also investigated similar strategies as a way to treat cystic fibrosis. Now, like colleagues around the world, McCray and He have both focused their research efforts on SARS-CoV-2, taking a similar tack to working with mouse models of infection and testing vaccines.
Finding an effective vaccine against the coronavirus that causes COVID-19 is a race against time, McCray said. "One hundred percent of the population is not going to be exposed to the virus the first time around, which means there will be more people to infect when it comes again," he said. "We don't know yet if people get lasting immunity from the SARS-CoV-2 infection, so it's important to think about ways to protect the population."
Source:
https://www.sciencedaily.com/releases/2020/04/200407072712.htm

Scheduled Server Maintenance and System Downtime Notice Dec 16, 2025
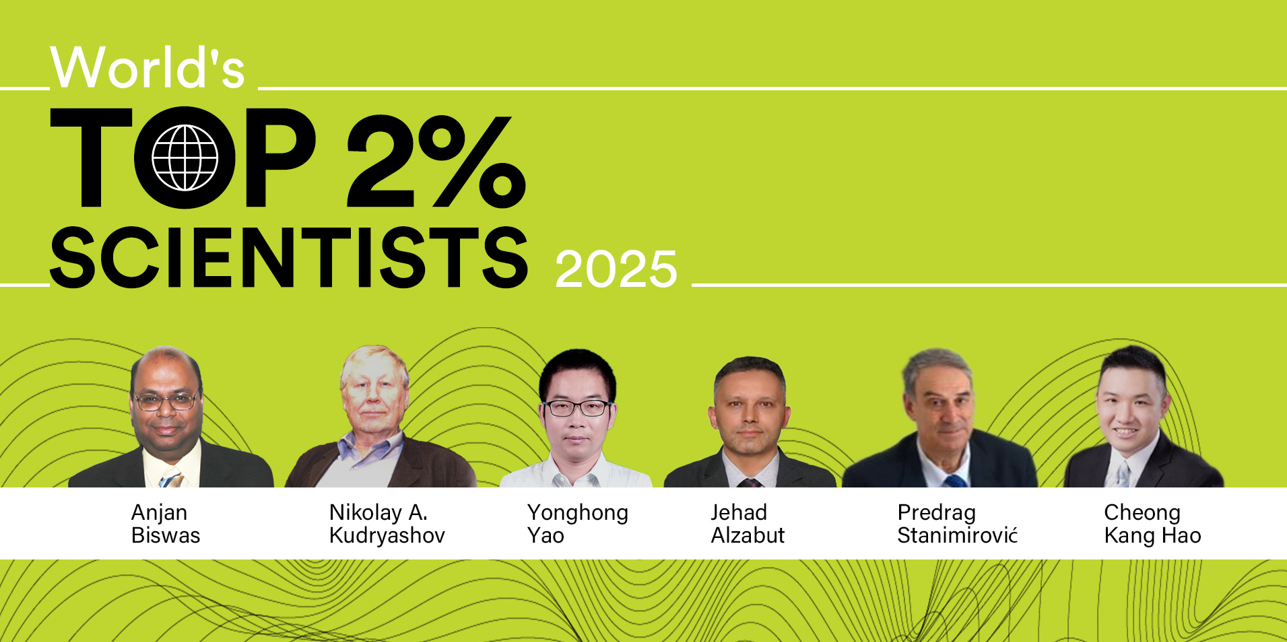
Celebrating CM Editorial Board Members Recognized in the Wor... Oct 10, 2025
Food Science and Engineering Now Indexed in CAS Database Aug 20, 2025
Contemporary Mathematics Achieves Significant Milestone in 2... Jun 19, 2025
Three Journals under Universal Wiser Publisher are Newly Ind... Apr 21, 2025